Hepatitis
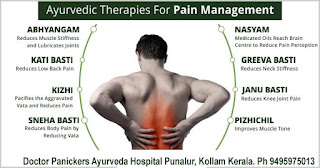
Kerala's Best Ayurveda HospitalDoctor Panickers Ayurveda Hospital Near Govt Higher Secondary School, Punalur, Kollam Kerala.Ph :09495975013, 09447775013
Hepatitis is an inflammation of the
liver, most commonly caused by a viral infection. There are five main hepatitis
viruses, referred to as types A, B, C, D and E, but it can also be caused due
to toxins (notably alcohol, certain medications, some industrial organic
solvents and plants), other infections and autoimmune diseases.
Hepatitis is acute when it lasts less
than six months and chronic when it persists longer. Some types of hepatitis
will pass without causing permanent damage to the liver. Other types can
persist for many years and cause scarring of the liver (cirrhosis) and, in the
most serious cases, loss of liver function (liver failure), which can be fatal.
In particular, types B and C lead to chronic disease in hundreds of millions of
people and, together, are the most common cause of liver cirrhosis and cancer.
Hepatitis A and E are typically
caused by ingestion of contaminated food or water. Hepatitis B, C and D usually
occur as a result of parenteral contact with infected body fluids. Common modes
of transmission for these viruses include receipt of contaminated blood or
blood products, invasive medical procedures using contaminated equipment and
for hepatitis B transmission from mother to baby at birth, from family member
to child, and also by sexual contact.
Acute infection may occur with
limited or no symptoms, or may include symptoms such as jaundice (yellowing of
the skin and eyes), dark urine, malaise or extreme fatigue, nausea, vomiting,
anorexia and abdominal pain.
Initial features are of nonspecific
flu-like symptoms, common to almost all acute viral infections and may include
malaise, muscle and joint aches, fever, nausea or vomiting, diarrhea, and
headache. More specific symptoms, which can be present in acute hepatitis from
any cause, are: profound loss of appetite, aversion to smoking among smokers,
dark urine, yellowing of the eyes and skin (i.e., jaundice) and abdominal
discomfort. Physical findings are usually minimal, apart from jaundice in a
third and tender hepatomegaly (swelling of the liver) in about 10%. Some
exhibit lymphadenopathy (enlarged lymph nodes, in 5%) or splenomegaly
(enlargement of the spleen, in 5%).
Acute viral hepatitis is more likely
to be asymptomatic in younger people. Symptomatic individuals may present after
convalescent stage of 7 to 10 days, with the total illness lasting 2 to 6
weeks.
A small proportion of people with
acute hepatitis progress to acute liver failure, in which the liver is unable
to clear harmful substances from the circulation (leading to confusion and coma
due to hepatic encephalopathy) and produce blood proteins (leading to
peripheral edema and bleeding). This may become life-threatening and
occasionally requires a liver transplant.
Chronic hepatitis often leads to
nonspecific symptoms such as malaise, tiredness and weakness, and often leads
to no symptoms at all. It is commonly identified on blood tests performed
either for screening or to evaluate nonspecific symptoms. The occurrence of
jaundice indicates advanced liver damage. On physical examination there may be
enlargement of the liver.
Extensive damage and scarring of
liver (i.e. cirrhosis) leads to weight loss, easy bruising and bleeding
tendencies, peripheral edema (swelling of the legs) and accumulation of ascites
(fluid in the abdominal cavity). Eventually, cirrhosis may lead to various
complications: esophageal varices (enlarged veins in the wall of the esophagus
that can cause life-threatening bleeding) hepatic encephalopathy (confusion and
coma) and hepatorenal syndrome (kidney dysfunction).
Acne, abnormal menstruation, lung
scarring, inflammation of the thyroid gland and kidneys may be present in women
with autoimmune hepatitis.
There are five main types of
hepatitis that are caused by a virus, A, B, C, D, and E.
The clinical presentation of
infectious hepatitis varies with the individual, as well as with the specific
causative virus. Some patients may be entirely asymptomatic or only mildly
symptomatic at presentation. Others may present with rapid onset of fulminant
hepatic failure (FHF). The classic presentation of infectious hepatitis
involves 4 phases, as follows:
§ Phase 1 (viral replication phase) – Patients are asymptomatic during
this phase; laboratory studies demonstrate serologic and enzyme markers of
hepatitis
§ Phase 2 (prodromal phase) – Patients experience anorexia, nausea,
vomiting, alterations in taste, arthralgias, malaise, fatigue, urticaria, and
pruritus, and some develop an aversion to cigarette smoke; when seen by a
health care provider during this phase, patients are often diagnosed as having
gastroenteritis or a viral syndrome
§ Phase 3 (icteric phase) – Patients may note dark urine, followed by
pale-colored stools; in addition to the predominant gastrointestinal (GI)
symptoms and malaise, patients become icteric and may develop right upper
quadrant pain with hepatomegaly
§ Phase 4 (convalescent phase) – Symptoms and icterus resolve, and liver
enzymes return to normal
This is caused by eating infected
food or water. The food or water is infected with a virus called HAV (Hepatitis
A Virus). Anal-oral contact during sex can also be a cause. HAV infection
usually occurs as a mild self-limited disease and confers lifelong immunity to
the virus. Nearly everyone who develops Hepatitis A makes a full recovery – it
does not lead to chronic disease.
The incubation period of hepatitis A
virus (HAV) is 2-7 weeks (average, 28 days). Clinical symptoms then develop,
often with a presentation similar to that of gastroenteritis or a viral
respiratory infection. The most common signs and symptoms include fatigue,
nausea, vomiting, fever, hepatomegaly, jaundice, dark urine, anorexia, and
rash.
This is an STD (sexually transmitted
disease). It is caused by the virus HBV (Hepatitis B Virus) and is spread by
contact with infected blood, semen, and some other body fluids. You get
Hepatitis B by:
Unprotected sexual intercourse with
an infected person (unprotected sex means without using a condom) Using a
syringe that was previously used by an infected person (most commonly happens
with drug addicts and people who inject steroids).
Having your skin perforated with
unsterilized needles, as might be the case when getting a tattoo, or being
accidentally pricked. People who work in health care risk becoming infected by
accident in this way. Sharing personal items, such as a toothbrush or razor,
with an infected person.
A baby can become infected through
his mother’s milk if she is infected.
Being bitten by someone who is
infected.
The incubation period for hepatitis B
virus (HBV) is 30-180 days (average, approximately 75 days). Patients then
enter the prodromal or preicteric phase, characterized by the gradual onset of
anorexia, malaise, and fatigue. During this phase, as the liver becomes
inflamed, liver enzymes start to elevate, and the patient may experience right
upper quadrant pain. About 15% of patients develop an illness resembling serum
sickness. These patients may experience fever, arthritis, arthralgias, or an
urticarial rash.
As the disease progresses to the
icteric phase, the liver becomes tender, and jaundice develops. Patients may
note that their urine darkens and that their stools lighten in color. Other
symptoms in this stage include nausea, vomiting, and pruritus.
From this point on, the clinical
course may be highly variable. Whereas some patients experience fairly rapid
improvements in their symptoms, others go on to experience prolonged disease
with slow resolution. Still others may have symptoms that periodically improve,
only to worsen later (relapsing hepatitis). Finally, there is an unfortunate
subset of patients in whom the disease rapidly progresses to FHF; this may
occur over days to weeks.
Hepatitis C is usually spread through
direct contact with the blood of a person who has the disease. It is caused by
the virus HCV (Hepatitis C Virus).
The incubation period for hepatitis C
virus (HCV) is 15-150 days, with symptoms developing anywhere from 5-12 weeks
after exposure. During acute HCV infection, symptoms may appear similar to
those of HBV infection. In up to 80% of cases, however, patients are
asymptomatic and do not develop icterus.
The liver can swell and become
damaged. In hepatitis C, unlike hepatitis B, liver cancer risk is only
increased in people with cirrhosis and only 20% of hep C patients get
cirrhosis. Feces is never a route of transmission in hepatitis C.
Only a person who is already infected
with Hepatitis B can become infected with Hepatitis D. It is caused by the
virus HDV (Hepatitis D Virus). Infection is through contact with infected
blood, unprotected sex, and perforation of the skin with infected needles. The
liver of a person with Hepatitis D swells.
The incubation period of hepatitis D
virus (HDV) is approximately 35 days. Patients simultaneously infected with HBV
and HDV often have an acute, self-limited infection. Fewer than 5% of these
patients develop chronic HDV infection.
Chronic HBV carriers who become
superinfected with HDV tend to have a more severe acute hepatitis; 80% of these
patients go on to develop chronic HDV infection. Chronic infection with HBV and
HDV may lead to fulminant acute hepatitis and severe chronic active hepatitis
with progression to cirrhosis. Over the long term, as many as 70-80% of these
patients have evidence of chronic liver disease with cirrhosis, compared with
only 15-30% of patients with chronic HBV alone.
A person can become infected by
drinking water that contains HEV (Hepatitis E Virus). The liver swells but
there is no long-term consequence. Infection is also possible through anal-oral
sex.
The incubation period of hepatitis E
virus (HEV) is 2-9 weeks (average, 45 days). No reports exist of chronic
infection with HEV.
Hepatitis can be caused by:
§ Immune cells in the body attacking the liver and causing autoimmune
hepatitis
§ Infections from viruses (such as hepatitis A, B, or C), bacteria, or
parasites
§ Liver damage from alcohol, poisonous mushrooms, or other poisons
§ Medications, such as an overdose of acetaminophen, which can be deadly
§ Liver disease can also be caused by inherited disorders such as cystic
fibrosis or hemochromatosis, a condition that involves having too much iron in
your body (the excess iron deposits in the liver).
§ Other causes include Wilson’s disease.
There are several laboratory tests
that may be used in cases of known or suspected hepatitis, including:
§ Abdominal ultrasound
§ Autoimmune blood markers
§ Hepatitis virus serologies
§ Liver function tests
§ Liver biopsy to check for liver damage
§ Paracentesis (if fluid is in your abdomen)
§ Detection of immunoglobulin M (IgM) for hepatitis A virus (HAV) is the
standard for diagnosing acute infection with HAV.
§ Detection of IgM for hepatitis B core antigen (HBcAg) in serum is
required to make the diagnosis of acute hepatitis B virus (HBV) infection.
Hepatitis B surface antigen (HBsAg) may be present in acute infection or in
patients who are chronic carriers. Its presence in patients with symptoms of
acute hepatitis strongly suggests acute HBV infection but does not rule out
chronic HBV with acute superinfection by another hepatitis virus. The presence
of HBsAg in the serum for 6 months or longer indicates chronic infection.
§ Hepatitis C virus (HCV) infection can be confirmed with serologic assays
to detect antibody to HCV (anti-HCV) or with molecular tests for the presence
of viral particles. Third-generation assays for anti-HCV are sensitive and
specific and can detect such antibodies within 4-10 weeks of infection. A rapid
antibody test strip has now been approved. Qualitative polymerase chain reaction
(PCR) assay for presence of viral particles is the most specific test of HCV
infection and may be helpful in diagnosing acute HCV infection before
antibodies have developed.
§ Assays to detect IgM antibody to hepatitis D virus (HDV) do not need to
be routinely performed in all patients with suspected hepatitis.
In general, complications of viral
hepatitis may include the following:
§ Acute or subacute hepatic necrosis
§ Chronic active hepatitis
§ Chronic hepatitis
§ Cirrhosis
§ Hepatic failure
§ Hepatocellular carcinoma (HCC) in patients with HBV or HCV infection
In Ayurveda, the
liver is called Yakrit. Pitta is the
predominant humor of the liver. Most liver disorders are aggravated conditions
of Pitta. Excessive bile production or a blockage in the flow of bile usually
indicates high pitta, which in turn affects the agni or enzyme activities
responsible for absorption, digestion and metabolism.
Aggravation of the Pitta causes the
liver diseases such as hepatitis, cirrhosis and fatty liver. Kaamala is the
term mentioned in Ayurveda to describe the wide range of liver diseases
including Hepatitis.
Ayurveda describes various types of
kaamala (hepatitis or jaundice) based on the stage or depth of the symptoms.
They are:
§ Shakhasrita – is caused by the aggravation of all the doshas (Vata, Pitta and
Kapha), and is a kind of obstructive jaundice.
§ Koshta shakhsrita – results from very high pitta derangement and considered as
severe jaundice or hepatitis, difficult to cure.
§ Kumbha kamala – is a neglected or untreated stage of jaundice or hepatitis. It
can become incurable if not attended immediately. It can be compared with
Cirrhosis of liver.
§ Haleemaka – is an advanced or neglected stage of Paandu roga that occurs
when both the vata and pitta are out of balance.
At Doctor Panickers Ayurveda Hospital
we are providing highly effective treatment for various type or Hepatitis
including hepatitis B & hepatitis C. Our treatment is useful in controlling
the infection & replication of the virus, preventing further damage to
liver. Hepatitis B patients show better response than Hepatitis C.
Our treatment involves Shodana
chikitsa (detoxification through Panchakarma procedures), Shamana chikitsa
(Palliative researched Ayurvedic medicines) and Kayakalpa (rejuvenation).
Diet restrictions, life style
modifications and de-addiction are also the essential factors practiced for the
best possible results.